- Glycine encephalopathy
-
Glycine Encephalopathy (Non-ketotic Hyperglycinemia) Classification and external resources 
GlycineOMIM 605899 MeSH D020158 Glycine encephalopathy (also known as non-ketotic hyperglycinemia or NKH) is a rare autosomal recessive disorder of glycine metabolism. After phenylketonuria, glycine encephalopathy is the second most common disorder of amino acid metabolism. The disease is caused by defects in the glycine cleavage system, an enzyme responsible for glycine catabolism. There are several forms of the disease, with varying severity of symptoms and time of onset. The symptoms are exclusively neurological in nature, and clinically this disorder is characterized by abnormally high levels of the amino acid glycine in bodily fluids and tissues, especially the cerebral spinal fluid.
Glycine encephalopathy is sometimes referred to as "nonketotic hyperglycinemia" (NKH), as a reference to the biochemical findings seen in patients with the disorder, and to distinguish it from the disorders that cause "ketotic hyperglycinemia" (seen in propionic acidemia and several other inherited metabolic disorders). To avoid confusion, the term "glycine encephalopathy" is often used, as this term more accurately describes the clinical symptoms of the disorder.
Contents
Pathophysiology
Glycine is the simplest amino acid, having no stereoisomers. It can act as a neurotransmitter in the brain, acting as an inhibitor in the spinal cord and brain stem, while having excitatory in the cortex of the brain. Glycine is metabolized to eventual end products of ammonia and carbon dioxide through the glycine cleavage system (GCS), an enzyme complex made up of four protein subunits. Defects in these subunits can cause glycine encephalopathy, although some causes of the disease are still unknown. The GCS has its highest activity levels in liver, brain and placental tissue. One of its main functions is to keep glycine levels low in the brain. Defects in GCS cause an increase of glycine concentration in plasma and cerebrospinal fluid.[1] The exact pathophysiology of the disorder is not known, but it is considered likely that buildup of glycine in the brain is responsible for the symptoms.[2]
All types on glycine encephalopathy show elevated levels of glycine in the plasma, and cerebral spinal fluid.[3] Glycine concentrations in the cerebrospinal fluid are typically more markedly elevated than in plasma, leading to a corresponding elevation in the ratio of glycine concentrations in the cerebral spinal fluid to that in the plasma. The ratio can also be slightly elevated if the patient is receiving valproic acid.[1]
Glycine encephalopathy (nonketotic hyperglycinemia) should not be confused with other metabolic disorders that can produce elevated glycine. For example, certain inherited 'organic acidurias' (aka 'organic acidemias') can produce elevated glycine in plasma and urine, although the disorders are not caused by defects in the glycine cleavage system.[4] Glycine encephalopathy is unique in the fact that levels of glycine are disproportionately elevated in CSF (in addition to blood and urine), whereas CSF glycine levels are normal or near-normal in patients with inherited organic acidurias.
Glycine metabolism
Glycine is metabolized in the body to end products of carbon dioxide and ammonia. The glycine cleavage system, which is responsible for glycine metabolism in the mitochondrion is made up of four protein subunits, the P-protein, H-protein, T-protein and L-protein.[1]
Classification
There are several different forms of glycine encephalopathy, which can be distinguished by the age of onset, as well as the types and severity of symptoms. All forms of glycine encephalopathy present with only neurological symptoms, including mental retardation, hypotonia, seizures and brain malformations.[1]
With the classical, or neonatal presentation of glycine encephalopathy, the infant is born after an unremarkable pregnancy, but presents with lethargy, hypotonia, seizures and myoclonic jerks, which can progress to apnea requiring artificial ventilation, and often death. Apneic patients can regain spontaneous respiration in their second to third week of life. After recovery from the initial episode, patients have intractable seizures and profound mental retardation, remaining developmentally delayed. Some mothers comment retrospectively that they noticed rhythmic hiccuping during pregnancy.[2] Patients with the infantile form of glycine encephalopathy do not show lethargy and coma in the neonatal period, but often have a history of hypotonia. They often have seizures, which can range in severity and responsiveness to treatment, and are typically developmentally delayed.[5] Glycine encephalopathy can also present as a milder form with episodic seizures, ataxia, movement disorders, and gaze palsy during febrile illness. These patients are also developmentally delayed, to varying degrees. In the later onset form, patients typically have normal intellectual function, but present with spastic diplegia and optic atrophy.[5]
Transient neonatal hyperglycinemia has been described in a very small number of cases. Initially, these patients present with the same symptoms and laboratory results that are seen in the classical presentation. The levels of glycine in plasma and cerebrospinal fluid normalize within eight weeks, and in five of six cases there were no neurological issues at follow-up times up to thirteen years. A single patient was severely retarded at nine months. An immature glycine cleavage system in the brain and liver is suspected as the cause of transient neonatal hyperglicinemia.[2]
Genetics
Glycine encephalopathy has an estimated incidence of 1 in 60,000, making it the second most common disorder of amino acid metabolism, after phenylketonuria. It is caused by a defect in the glycine cleavage system (GCS), which is made up of four protein subunits. Each of these four subunits is encoded by a separate gene. Defects in three of these four genes have been linked to glycine encephalopathy.[1]
Gene Name Percent GLDC encodes the "glycine dehydrogenase" subunit, also called "glycine decarboxylase" About 70-75% of cases of glycine encephalopathy result from mutations in the GLDC gene. GCST or AMT encoding the "aminomethyltransferase" subunit About 20% of cases are caused by mutations in the AMT gene. GCSH encoding the subunit "glycine cleavage system protein H" Mutations in the GCSH gene account for less than 1% of cases. There is a fourth unit in the complex, dihydrolipoamide dehydrogenase or GCSL. However, to date there have been no mutations in GCSL found to be associated with glycine encephalopathy.
A small percentage of affected individuals do not have a detectable mutation in any of the three genes (listed above) but still have defective glycine-cleavage enzymatic activity. It is thought that these patients may have mutations in the genes encoding one of the cofactors associated with the GCS complex.
Defects in the GSC proteins can prevent the complex from functioning properly or can prevent the GCS complex from forming entirely. When the complex is unable to break down glycine properly, this causes excess glycine to build up to toxic levels in the body's organs and tissues. Damage caused by harmful levels of glycine in the brain and cerebrospinal fluid is responsible for the characteristic seizures, breathing difficulties, movement disorders, and mental retardation.
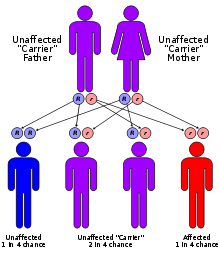
This disorder is inherited in an autosomal recessive pattern. The term "autosomal" signifies that the gene associated with the disorder is located on an autosome. In an autosomal recessive inheritance pattern, two defective copies of the gene (one inherited from each parent) are required in order for a child to be born with the disorder. Therefore, each parent of an individual with an autosomal recessive disorder has at least one defective copy of the gene. With autosomal recessive disorders, individuals with only one copy of a defective gene (heterozygotes) are considered "carriers" for the disorder. Carriers usually do not show signs or symptoms of the disorder.[6]
See also
- List of amino acid metabolism disorders
- inborn errors of metabolism
References
- ^ a b c d e Sarafoglou, Kyriakie; Hoffmann, Georg F.; Roth, Karl S., eds. Pediatric Endocrinology and Inborn Errors of Metabolism. New York: McGraw Hill Medical. p. 811.
- ^ a b c "Nonketotic hyperglycinemia". McGraw Hill. http://www.ommbid.com/OMMBID/the_online_metabolic_and_molecular_bases_of_inherited_disease/b/abstract/part8/ch90. Retrieved 2011-09-22.
- ^ Sarafoglou, Kyriakie; Hoffmann, Georg F.; Roth, Karl S., eds. Pediatric Endocrinology and Inborn Errors of Metabolism. New York: McGraw Hill Medical. p. 793.
- ^ "The Organic Acidemias: An Overview -- GeneReviews -- NCBI Bookshelf". http://www.ncbi.nlm.nih.gov/bookshelf/br.fcgi?book=gene&part=oa-overview.
- ^ a b "Glycine Encephalopathy". National Center for Biotechnology Information, U.S. National Library of Medicine. http://www.ncbi.nlm.nih.gov/books/NBK1357/. Retrieved 2011-09-22.
- ^ "Autosomal recessive: MedlinePlus Medical Encyclopedia". http://www.nlm.nih.gov/medlineplus/ency/article/002052.htm.
Inborn error of amino acid metabolism (E70–E72, 270) K→acetyl-CoA Lysine/straight chainHypertryptophanemiaG G→pyruvate→citrateG→glutamate→
α-ketoglutarateGlutamate/glutamineG→fumarateType II tyrosinemia · Type III tyrosinemia/Hawkinsinuria · Alkaptonuria/Ochronosis · Type I tyrosinemiaTransport/
IE of RTTOther Categories:- Amino acid metabolism disorders
- Inborn errors of metabolism
- Autosomal recessive disorders
Wikimedia Foundation. 2010.